Sexually transmitted diseases (STDs) are a common health problem today. Among these diseases, there are two important infections that are often confused: Molluscum Contagiosum and Condyloma. Although they are both viral infections that cause skin lesions, there are important differences between them. In this blog post, we will explore in detail the main differences between Molluscum Contagiosum and Condyloma.
Causative Viruses and Transmission Routes
Molluscum Contagiosum
Molluscum Contagiosum is a skin infection caused by Molluscum Contagiosum Virus (MCV) from the Poxviridae family. This virus has four different subtypes: MCV-1, MCV-2, MCV-3 and MCV-4. The most common of these subtypes is MCV-1.
Transmission Routes
The transmission routes of Molluscum Contagiosum are as follows:
- Direct skin contact
- Sexual contact
- Sharing contaminated items (towels, clothes, etc.)
- Yüzme havuzları ve saunalar gibi nemli ortamlar
It is especially common in children and people with weak immune systems.
Condyloma
Condyloma, also known as genital warts, is a sexually transmitted disease caused by Human Papillomavirus (HPV). There are more than 200 types of HPV, but the types that cause genital warts are usually HPV-6 and HPV-11.
Transmission Routes
The main ways condyloma is transmitted are:
- Sexual contact (vaginal, anal or oral)
- From mother to baby during labor
- Rarely, contact with contaminated surfaces
Condyloma can occur in sexually active people of any age.
Clinical Signs and Symptoms
Molluscum Contagiosum
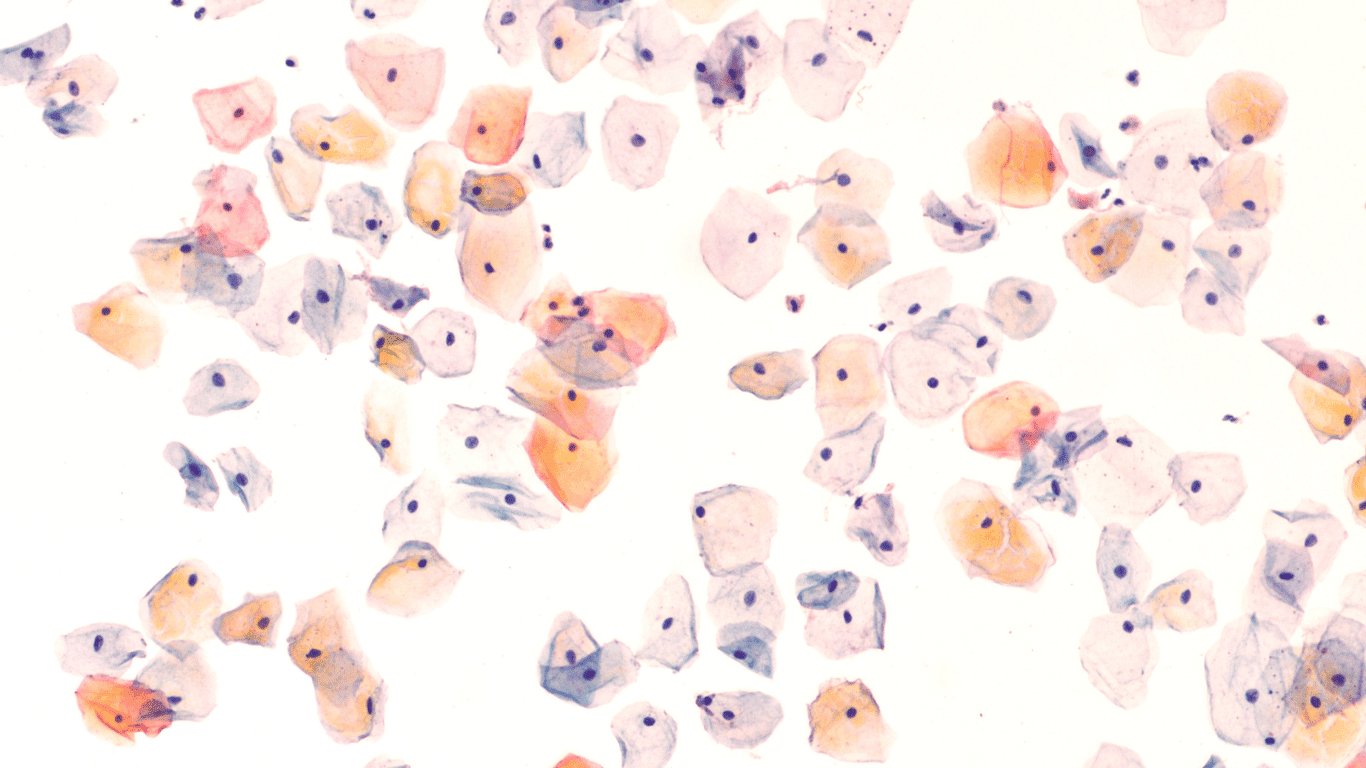
The characteristic features of Molluscum Contagiosum are the following:
- Small, round and shiny lesions
- Usually 2-5 mm in diameter
- Bellied look in the middle
- Tan or slightly pink in color
- Usually painless and itchless
Settlements
Molluscum Contagiosum lesions can appear anywhere on the body, but the most common sites are
- Body
- Armpits
- Elbow pits
- Groin area
- Genital area (in adults)
Condyloma
These are the characteristic features of condyloma:
- Small, flesh-colored or brownish projections
- Can grow in cauliflower appearance
- Can be single or multiple
- Sometimes it may cause itching or burning sensation
- Rarely can be painful
Settlements
Condyloma lesions usually occur in the following areas:
- Genital area (penis, vagina, vulva)
- Around the anus
- Intraoral (in case of transmission through oral sex)
Diagnostic Methods
Molluscum Contagiosum
Molluscum Contagiosum is usually diagnosed by clinical examination. Due to their characteristic appearance, they can be easily diagnosed by an experienced physician. However, the following methods can be used for definitive diagnosis:
- Dermoscopy: Allows more detailed examination of lesions.
- Biopsy: In rare cases, a sample of the lesion may be taken and examined to confirm the diagnosis.
- Polymerase Chain Reaction (PCR): Can be used to detect the genetic material of the virus.
Condyloma
The following methods can be used to diagnose condyloma:
- Clinical examination: An experienced physician can diagnose genital warts visually.
- Acetic acid test: Acetic acid applied to the suspicious area makes the lesions more visible.
- Biopsy Can be used for definitive diagnosis and to determine the type of HPV.
- HPV DNA test: Used to determine the presence and type of virus.
Treatment Approaches
Molluscum Contagiosum
Molluscum Contagiosum is an infection that usually heals on its own. However, treatment can be applied to prevent spread and address aesthetic concerns. Treatment options include:
- Cryotherapy Removal of lesions by freezing
- Curettage Removal of lesions by scraping
- Topical medicines:
- İmichimod cream
- Podophyllotoxin solution
- Kantaridin
- Oral antivirals: Can be used in immunocompromised patients
Treatment Duration and Follow-up
Treatment for Molluscum Contagiosum usually takes a few weeks to several months. Regular check-ups are important during treatment. New lesions may develop and additional treatment may be needed.
Condyloma
Condyloma treatment may vary depending on the size, number and location of the lesions. Treatment options include:
- Topical treatments:
- İmichimod cream
- Podophyllotoxin solution
- Synechatechins
- Cryotherapy
- Electrocoter
- Laser treatment
- Surgical excision
- Immunomodulatory therapies
Treatment Duration and Follow-up
Condyloma treatment usually takes a few weeks to a few months. Because of the high risk of recurrence, regular check-ups are recommended for at least 6 months after treatment.
Complications and Long-Term Effects
Molluscum Contagiosum
Molluscum Contagiosum usually does not cause serious complications. However, in some cases the following problems may occur:
- Secondary bacterial infections
- Permanent scarring of the skin (rare)
- Eye infections (in eyelid lesions)
- Psychological effects (especially in children and adolescents)
Long Term Prognosis
Molluscum Contagiosum is usually a benign infection and in most cases resolves spontaneously within 6-12 months. Long-term negative effects are rare in people with normal immune systems.
Condyloma
The potential complications and long-term effects of condyloma can be more serious:
- Cancer risk: Some HPV types (especially 16 and 18) can cause cancers of the cervix, anus, penis and oropharynx.
- Birth complications: During pregnancy, genital warts can grow and block the birth canal.
- Psychological effects: Sexual dysfunction, depression and anxiety may develop.
- Recurrence There is a high risk of recurrence after treatment.
Long Term Prognosis
The long-term prognosis of condyloma depends on the type of HPV and the immune status of the person. Regular follow-up and early intervention are important to prevent possible complications.
Prevention Methods
Molluscum Contagiosum
The following measures can be taken to prevent Molluscum Contagiosum:
- Paying attention to personal hygiene
- Avoid direct contact with infected people
- Not sharing common items (towels, clothes, etc.)
- Being careful in humid environments such as swimming pools and saunas
- Using condoms to prevent sexual transmission
Condyloma
The following measures can be taken to prevent condyloma:
- HPV vaccination (recommended between the ages of 9-26)
- Practicing safe sexual intercourse (condom use)
- Regular gynecological/urological check-ups
- Not smoking (can accelerate the progression of HPV infection)
- Strengthen the immune system
Social Impacts and Awareness
Molluscum Contagiosum
Because Molluscum Contagiosum is particularly prevalent among children, it can be a major health concern in schools and public places. Community awareness raising efforts should include:
- Training programs for parents and teachers
- Strengthening hygiene practices in schools
- Work to prevent stigmatization of infected children
Condyloma
Condyloma is an important social problem in sexual and reproductive health. Awareness raising efforts should include:
- Comprehensive sex education programs
- Scaling up the HPV vaccine
- Promoting regular screening programs
- Reducing social stigma around sexually transmitted diseases
Conclusion
Molluscum Contagiosum and Condyloma, although both viral infections, differ significantly in their causative viruses, transmission routes, clinical manifestations, treatment approaches and long-term effects. While Molluscum Contagiosum is a relatively harmless infection that usually heals on its own, Condyloma can lead to more serious health problems and requires long-term follow-up.
Increasing public awareness, regular health checks and safe sexual practices are essential for the prevention and effective management of both infections. Healthcare professionals should know the distinctive features of these two infections and provide their patients with the right diagnosis and treatment approaches.
In conclusion, knowledge about Molluscum Contagiosum and Condyloma is critical to protect our personal health and contribute to public health. If you have any suspicion about these infections, it is important to contact a healthcare provider immediately.